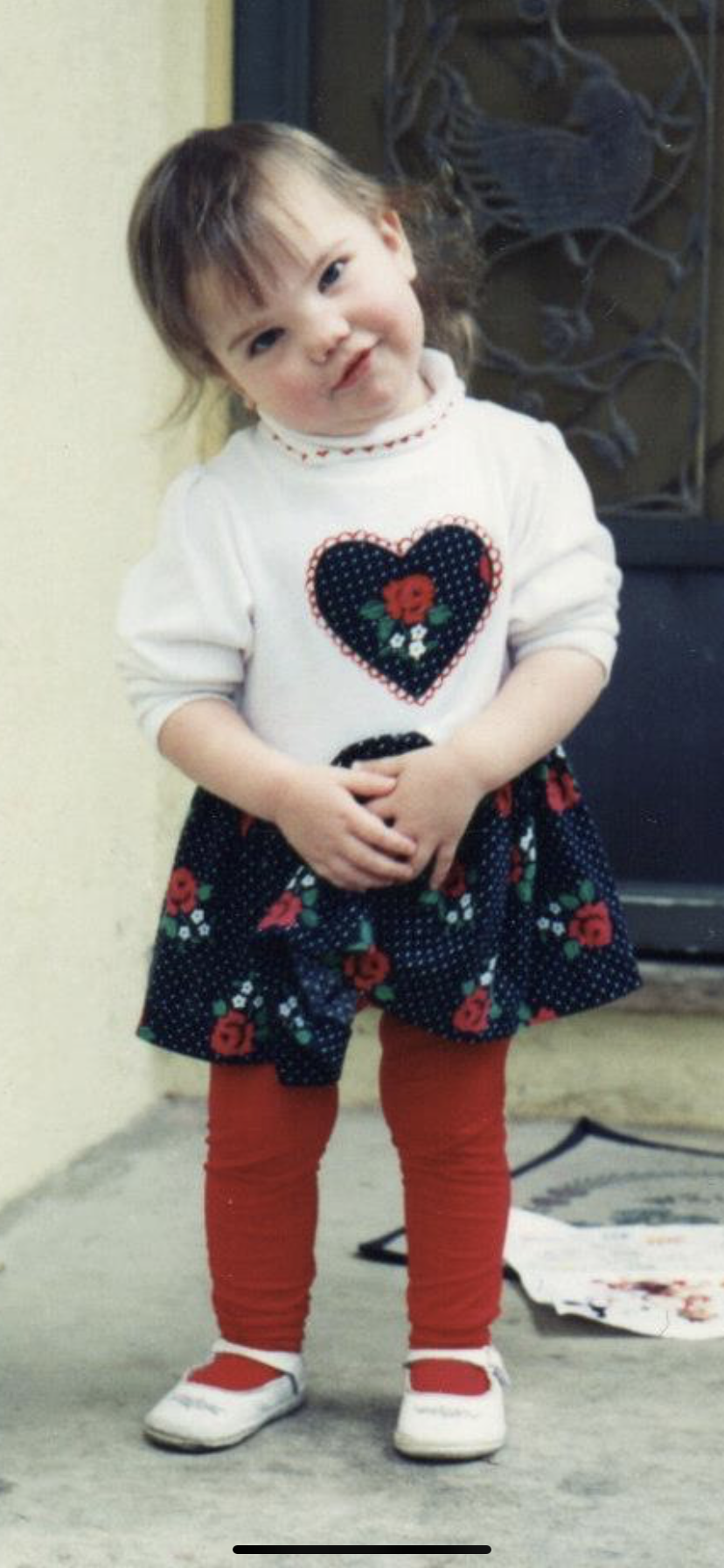
Q: Was it present/obvious in childhood?
A: Looking back, you can see how odd the positioning of my knees was as far back as baby pictures. It’s clearly congenital. I always had trouble with my ankles, but I was an active kid and we assumed it was damage from figure skating or karate or whichever other high impact activity I was involved in at the time. I began to physically struggle more obviously in high school, but was dismissed by several non-specialist doctors. The degradation sped up and culminated in needing a cane by age 24.
Pictured below: 1992 vs. 2009ish.
Q: How did you get diagnosed/who did you see first?
A: When it became clear I was consistently losing mobility and it wasn’t a temporary problem, I went to my primary care physician who said verbatim, “I have literally never seen something like this before.” She sent me to a sports-centric orthopedic surgeon, who brought a handful of physicians into the room to gawk at me before referring me yet again to a specialist at Boston Children’s Hospital. I was just barely under the age 25 cutoff to be seen there and Dr. Snyder gave me a confident diagnosis during our first appointment.
What I Wish I Had Known: Typically, MMS is diagnosed in children and it’s much less commonly addressed in adults. Hopefully that’s changed a bit since I was searching for a physician. It was very difficult to find a specialist who was both knowledgeable about MMS and was also willing to see me due to age. Most of the providers I found were pediatric and wouldn’t take me as a patient, but their offices were a good avenue to source word-of-mouth recommendations to appropriate surgeons. Regardless of where you start your diagnostic journey, you’ll ultimately need to see an orthopedic surgeon and the more specialized, the less time you’ll spend feeling frustrated, ignored, and gaslit.